StudentShare


Our website is a unique platform where students can share their papers in a matter of giving an example of the work to be done. If you find papers
matching your topic, you may use them only as an example of work. This is 100% legal. You may not submit downloaded papers as your own, that is cheating. Also you
should remember, that this work was alredy submitted once by a student who originally wrote it.
Login
Create an Account
The service is 100% legal
- Home
- Free Samples
- Premium Essays
- Editing Services
- Extra Tools
- Essay Writing Help
- About Us
✕
- Studentshare
- Subjects
- Health Sciences & Medicine
- The Neurophysiology of Peripheral Neurogenic Pain
Free
The Neurophysiology of Peripheral Neurogenic Pain - Essay Example
Summary
From the paper "The Neurophysiology of Peripheral Neurogenic Pain" it is clear that the pain pathway includes Nociceptors and primary and secondary afferent fibers. Other forms of pain include Nociceptive pain, Central sensitization, and Neurogenic pain. …
Download full paper File format: .doc, available for editing
GRAB THE BEST PAPER92.4% of users find it useful
- Subject: Health Sciences & Medicine
- Type: Essay
- Level: Undergraduate
- Pages: 17 (4250 words)
- Downloads: 0
- Author: quintenlittle
Extract of sample "The Neurophysiology of Peripheral Neurogenic Pain"
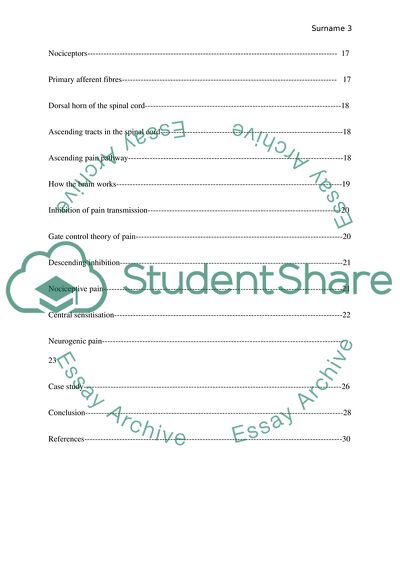
The Neurophysiology of Peripheral Neurogenic Pain Contents Epidemiology of pain ----------------------------------------------------------------------------------- 7
Differences in pain Levels------------------------------------------------------------------------------ 7
Differences of pain levels according to Gender and age------------------------------------------- 7
Differences of pain levels according to level of income------------------------------------------- 8
Differences of pain levels according to occupation----------------------------------------------- 10
Differences of pain levels according to race------------------------------------------------------- 12
Adjustable aspects associated with pain------------------------------------------------------------ 13
Types of pain------------------------------------------------------------------------------------------- 13
Acute pain---------------------------------------------------------------------------------------------- 14
Chronic pain------------------------------------------------------------------------------------------- 15
Nocigenic, Behavioural, Neurogenic, psychogenic, and paradoxical pain ------------------- 15
Classification of pain----------------------------------------------------------------------------------- 16
Classification according to duration------------------------------------------------------------------ 16
Classification according to medical perspective---------------------------------------------------- 17
Classification according to severity----------------------------------------------------------------- 17
Pain pathway mechanisms---------------------------------------------------------------------------- 17
Nociceptors--------------------------------------------------------------------------------------------- 17
Primary afferent fibres-------------------------------------------------------------------------------- 17
Dorsal horn of the spinal cord-------------------------------------------------------------------------18
Ascending tracts in the spinal cord--------------------------------------------------------------------18
Ascending pain pathway--------------------------------------------------------------------------------18
How the brain works------------------------------------------------------------------------------------19
Inhibition of pain transmission------------------------------------------------------------------------20
Gate control theory of pain-----------------------------------------------------------------------------20
Descending inhibition-----------------------------------------------------------------------------------21
Nociceptive pain-----------------------------------------------------------------------------------------21
Central sensitisation-------------------------------------------------------------------------------------22
Neurogenic pain------------------------------------------------------------------------------------------23
Case study------------------------------------------------------------------------------------------------26
Conclusion------------------------------------------------------------------------------------------------28
References------------------------------------------------------------------------------------------------30
List of figures
Figure 1: Age-Sex frequency of pain situations in Seattle, WA------------------------------------8
Figure 2: Commonness of migraines according to economic status in the US in people aged 12-80 years.---------------------------------------------------------------------------------9
Figure 3: Commonness of lower back pains according to level of education in the US in individuals above the age of 25-------------------------------------------------------------- 11
Figure 4: The types of pain---------------------------------------------------------------------------- 15
Figure 5: Ascending pathway------------------------------------------------------------------------- 20
Figure 6 How Pain works------------------------------------------------------------------------------ 21
Figure 7 Transmission of Nociceptive pain--------------------------------------------------------- 23
Figure 8 The role of central sensitization------------------------------------------------------------ 24
Figure 9 Neurogenic pain------------------------------------------------------------------------------ 25
Figure 10 Trapped nerve------------------------------------------------------------------------------- 29
List of tables
Table 1: Limitations in activity contributed by chronic back pain according to level of income in 1997----------------------------------------------------------------------------------10
Table 2: locations prevalence, persistency, and effects---------------------------------------------11
Table :3 Prevalence of headache, low back pain, and neck pain in the US in 2011------------13
Table 4: Difference between Nociceptive and Neurogenic pain--------------------------------- 16
Table 5: Distinguishing features of primary afferent fibres----------------------------------------18
Epidemiology of pain
Since time immemorial, people have always experienced painful episodes in various parts of the body. Virtually, human beings can experience pain in every part of the body. Sofaer defines pain as "An unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage" (p. 15).1 In laymans terms, pain can be described as physical uneasiness, anguish, and affliction arising from tissue damage or disease. This paper focuses on all the aspects of peripheral Neurologic pain. The epidemiology of pain can be addressed through paying much attention on widespread and intermittent pain disorders. In focusing on the epidemiology of pain, then a question arises whether persistent pain is a result of unremitting or never-ending ailment.2
Though diseases are caused by a wide range of factors, pain on the other hand can be as a result of a lone factor such as tissue damage or harm.3 What differs in terms of pain is the extent, amount or strength, and scale. The term scale in this aspect denotes that pain may either be bodily, emotional, or mental. Subsequently, individual views or opinions regarding pain also differs.3
Differences in pain levels
Differences of pain levels according to Gender and age. The frequency of pain is higher in women as compared to men.4 This factor is attributed to genetic differences between male and female, and also responsibilities bestowed on each gender by the society. This means that women are more prone to pain since their forbearance is minimal. The following graph illustrates the differences on frequency or commonness of pain among men and women:
Figure 1: Age-Sex frequency of pain situations in Seattle, WA.2
Percentage (y-axis)
Age (x-axiS)
According to Hecke, Torrance and Smith, Medical records in health institutions have shown a higher proportion of women seeking treatment for pain related problems as compared to men..5 However, pain differences in regard to gender goes hand in hand with age (Figure 1). This graph shows that pain is higher for women between the age of eighteen to forty four. This is attributed to elevated levels of hormones among women at this age.5 After attaining the age of forty four, pain drops significantly as this is the average age women undergo menopause.5 Hecke, Torrance, and Smith also assert that chronic pain becomes more common and severe and an individual advances in terms of age.5
Differences of pain level according to level of income. There are also other factors associated with pain such as the place of origin. Pain is more prevalent in third world countries as compared to developed nations based on the fact that developed nations have more advanced health care systems.6 In most cases, conditions that may elevate the intensity of pain in developing countries may go unattended hence increase in severity. Available sources also indicate that the commonness of pain as well as the intensity is largely dependent on the socio-economic status of individuals. Higher socio-economic class means that people have access to appropriate facilities necessary for pain management. Individuals in higher socio-economic class are also able to afford high quality health care.6 Western countries are associated with lower incidences of pain occurrences as compared to other countries.6 Similarly, this is attributed to the fact that Western countries have better strategies put into place to ensure individual pain management at all levels. These countries also have better political systems as compared to developing nations. Health care is dependent on the political situations of a country hence the differences in pain occurrences between countries.
Figure 2: Commonness of migraines according to economic status in the US in people aged 12-80 years. 2
percentage (y)
Gender (x axis)
This graphical representation of frequency of pain shows that the lower the level of income, the higher the incidence or commonness. The prevalence of pain based on the level of income can also be illustrated through elucidating how pain limits individual activity levels as shown below:
Table 1: Limitations in activity contributed by chronic back pain according to level of income in 1997.6
Adults age 18 years and above
Activity limitations due to Chronic back conditions (per 1000 people)
Poor people
77 people
Near poor people
53 people
Middle/High income people
24 people
Occupation. Prevalence of pain is also determined by individual occupation. Pain may be caused by work related factors such as the market dynamics. For instance, workers are more likely to suffer from migraines when market conditions are dire.7 Employees are therefore more likely to fail to report to the office depending on the severity of the pain. According to Schultz and Gatchel, the type of work is determined by the individuals level of education.7 In my opinion, Back pains are more likely to be experiences by individuals with high school education as compared to individuals who have attained post graduate degrees. This is attributed to the fact that more learned individuals are given supervisory roles in the workplace while those who have attained high school level education are involved in physical and more challenging roles in the workplace.8
Commonness of lower back pains according to level of education in the US in individuals above the age of 25 (n=10,404) in percentage
Figure 3: Commonness of lower back pains according to level of education in the US in individuals above the age of 25. 2
Percentage (Y-axis)
Level of education (x-axis)
In delineating the epidemiology of pain, it would also be important to illustrate locations in the human body prone to pain, its persistency, as well as it effect. Available sources have posited that more people have complained of headaches all over the world as compared to other locations in the body.9 Pain in the ankles and foot are the least common sources of pain as shown in the table below:
Table 2: Pain locations prevalence, persistency, and effects.2
LOCATION
PRVLENCE
DURATION >3 MONTHS
OCCURS ON HALF DAYS+
HIGH IMPACT ON ACTIVITIES
HEADACHE
40%
66%
16%
11%
ABDOMINAL
23%
67%
30%
18%
BACK
39%
81%
45%
32%
NECK
31%
81%
47%
32%
SHOULDER
29%
79%
51%
33%
HAND/WRIST
23%
77%
52%
37%
HIP/KNEE
28%
83%
55%
40%
ANKLE/FOOT
17%
80%
61%
42%
Differences of pain levels according to Race. Ethnicity contributes significantly on the increased incidences of pain. In the US for example, Blacks and other minority groups report increased cases of pain.10 This can be as a result of a number of reasons. This may be as a result of prejudice and cultural obstacles that limits the ease of access to health care facility. Individual views and opinions towards health also differ depending on cultural beliefs of each ethnic group. For instance, individuals with Asian backgrounds tend to fear the consequences of using pain relieving medicines more than the pain itself.11 Other ethnic groups such as the whites would prefer to use medication to alleviate the pain instead of worrying about the consequences.12 The following table shows pain levels and occurrences according to race according to National Centre for Health Statistics:
Table 3: Prevalence of headache, low back pain, and neck pain in the US in 2011.11
Race
Severe Headaches or Migraines
Low back pain
Neck pain
Whites only
16.9%
29.0%
15.6%
Black/African American
17.2%
27.6%
13.0%
Hispanic or Latino
16.1%
27.4%
14.7%
American Indian or Alaska Native Only
21.5%
31.0%
16.6%
Asian only
11.4%
19.8%
10.6%
Two or more races
19.5%
37.6%
20.2%
Adjustable aspects associated with pain. Some causes of pain are adaptable, meaning they can be prevented. One of these causes include psychological causes of pain such as depression and stress. Pain is also associated with other underlying medical condition.13 For instance, pain may be as a result of heart related ailments. According to Hecke, Torrance and Smith, "There is evidence that several chronic conditions may increase the risk of chronic pain through increased nociception from the periphery, resulting in central and peripheral pathophysiological changes associated with chronic pain".5 In addition, this may occur as a result of elevated levels of stress that may lead to the collapse of muscles and other tissues in the body. Smoking and alcoholism increases the prevalence of pain.14 Other factors that elevates the incidences of pain include lifestyle diseases such as obesity, erroneous physical activity and exercises lack of enough sleep, and poor nutrition.15
Types of pain
According to Hardy and Hardy, there are two main types of pain. Each of these two types of pains is also divided into four other types of pain in each on them. It is important to consider the fact that these types of pains are clustered based on their reaction to the various modes of management. In essence, there is a single type of pain present though sometimes there may be a second type of pain at any given time.16 In outlining the types of pain, Hardy and Hardy asserts that:
The two main types of pain are those of acute and chronic pain. These are the types of pain not a measure of the degree of pain. There are four further subtypes of pain- Nocigenic, Behavioural, Neurogenic, and psychogenic. The separate sub grouping is of Paradoxical pains.16
Figure 4: The types of pain.17
Acute pain .Acute pain is defined as the pain that takes place instantaneously when there is damage to body tissue or when a medical condition arises.4 For instance, pain felt on the leg or hand after a bone fracture is considered an acute pain. Hardy and Hardy puts across the fact that in many cases, this type of pain continues until the end of the therapeutic or curative procedure, and this may be up-to three months.4 However, this pain is not continuous and may be felt only when the injured part of the body is disturbed. This type of pain is closely linked with the discharge of specific chemical elements that functions to hearten and persuade immobility or apathy geared towards permitting and fastening recuperation.16
Chronic pain .Bono defines chronic pain as a type of pain that continues even after recuperation and may exceed by up-to one month..18 Since this pain takes place after acute pain, it is linked with an individuals attempt to move the part of the body that was motionless or static during acute pain period. Therefore, the individual may not be prepared both physically and mentally to provoke movement. Therefore, an individual is rendered motionless. In fact, this type of pain is believed to be as a result of misery due to changes in normal functioning of the body.19
Nocigenic pain, Behavioural, Neurogenic, psychogenic, and paradoxical pain. This type of pain is linked to the arousal or activation of the typical and well established conduit or course of pain starting from the tangential protein molecules located within or on the outer surface of a cell that obtains signals from the cell. It is important to expound on the verity that this type of pain is felt at the preliminary phase of a tissue damage or when a sickness arises. Behavioural pain is a type of pain that commences ass a Nocigenic pain that later cause a transformation in terms of behaviour. Neurogenic pain, on the other hand, is a type of pain that is felt as a result of injury to the nervous system tangentially or internally. Hardy and Hardy posits that psychogenic pain is a type of pain that arises as a type of psychological infirmity.16 Paradoxical pain is defined as pain resulting from all other types of pain and it is exacerbated by painkillers.20 The following shows the difference between Nocigenic (Nociceptive) and Neuropathic (Neurogenic) pains.21
Table 4: Difference between Nociceptive and Neurogenic pain.21
Classification of pain
In elucidating the classification of pain, it is of significance to posit that pain is a multifaceted course of action that can be classified in a number of ways. According to Sinatra, Jahr and Watkins-Pitchford, pain is classified according to period or length, greatness, means, medical situations and perspective.22 According to its greatness, pain is further classified into "mild, moderate, and severe".23 According to its length or extent, pain is further categorised into "acute, convalescent, and chronic"22. According to its means, pain is classified into "physiological, Nociceptive, and neuropathic" (Watkins 3), and according to its medical perspective, pain is classified into "post-surgical, malignancy-related, neuropathic, and degenerative".22 Some of these modes of classification will be discussed below. However, there are also other modes of classification of pain such as classification founded on functioning, and classification on the basis of its cause.24
Classification in terms of length/duration. This is considered one of the universal methods or technique of pain classification. At this level, pain is either acute, or chronic. General examples of acute pain (as mentioned earlier) may include injury to the body tissues, irritation as a result of soreness, and ailments with short intervals. Chronic pain on the other hand goes on for a long time.25
Classification in terms of medical perspective. This mode of classification focuses on the part of the body affected by the pain. Practically every part of the body can experience pain. Some of the most common ones include migraines and back pains. In categorising pain in this perspective, the part of the body where pain warning signs are prevalent is identified.24
Classification according to severity. Pain is also classified depending on its ruthlessness. In doing this, a range of values are used from zero to ten. A range of zero denotes the absence of pain while a range of ten denotes the most severe pain. However, this mode of classification may produce skewed results due to the fact that personal or individual accounts, details, and descriptions used to classify the pain.24
Pain pathways and mechanisms
One of the roles of pain in the body is that it helps prevent injury through firing warning signals, and it involves body senses as well as mental conditions of the body.26
Nociceptors. These are defined as specific sensory nerve endings with the capacity to retort to either peripheral stimuli or from a stimuli originating from the inside of the body.26 These nerve endings are used to sense and identify repulsive occurrences that induce precise responses within an organ or body tissue. These repulsive occurrences are then transmitted into either the brain or the spinal cord for as electrical currents for processing. When the skin or any other part of the body is injured, the body discharges seditious elements that leads to swelling.26 A good example of these elements include cytokines and serotonin.
Primary afferent fibres. These are beta amyloid threads or filaments whose main objective is to transport non-toxic or non-lethal stimulus. Others include delta fibres, and group C nerve fibres.26 These three types of fibres have are different in terms of size, speed of transmission, and sense as shown in the table below:
Table 5: Distinguishing features of primary afferent fibres.26
Feature
Amyloid-beta
Amyloid delta
C nerve fibres
width
big
tiny
least
Myelination
very
lightly
Not myelinated
Speed of transmission
Less than 40ms-1
5 to 15 ms-1
Less than 2 ms-1
Receptor activation thresholds
short
Both short and soaring
soaring
Sensation on stimulation
Light touch, non toxic
Fast and razor-sharp pain restricted to a small area
Sluggish, distributed, and tedious pain
Dorsal horn of the spinal cord. Lewis et-al brings forward the fact that the amyloid-delta together with group C nerve fibres allow the transmission of electric signals or currents from the nerves into the cells in the dorsal horn of the spinal cord. At this region, there are composite and intricate communications taking place involving afferent neurons, interneuron, as well as other conduits or courses.26 It is important to posit that these communications involving these neurons are the decision makers on the actions carried by the secondary afferent neurons.26
Ascending tracts in the spinal cord. Ascending tracts are the pathways hat transmit or relay Nociceptive signals towards the brain for processing.27 There are two courses involved in this process. These signals are transmitted through spinothalamic and spinoreticular strips. In the spinothalamic strip, secondary afferent neurons are involved in the transmission process as they originate from the spinal cord into the brain. This strip only transmits electric signals significant for the containment of the twinge or hurting. In the spinoreticular strip, threads intersect and crisscross each other and then rise parallel to arrive at the posterior part of the brain. From the posterior part of the cerebrum, these strands extend further into the thalamus, hypothalamus, and into the remotest and encrusted structure of neurons in the cerebrum.27 In comparison to the spinothalamic strip, the spinoreticular strip is concerned with expressive or sentimental features of ache or hurting.27
Figure 5: Ascending pathway.28
How pain is processed in the brain. Pain is considered a very intricate and multifarious occurrence influenced by various aspects such as individuals disposition, conviction, as well as heredity issues.29 The containment and limitation of the feeling of pain is achieved by the somatosensory cortex. Past research and experiments have elucidated the fact that a complex system of the cerebrum is stimulated during the pain process.29 During this process, both the major and minor somatosensory are stimulated. Others parts of the cerebrum stimulated during this process include the cortex and the thalamus.29 The figure below shows how pain is processed in the cerebrum.
Figure 6: How Pain works.30
Inhibition of pain transmission. As mentioned above, the process of pain is an intricate one. This is also attributed to the fact that there are additional processes in action with the sole and main function of hindering or slowing down the communication or conduction of pain when it reaches the spinal cord.31 In fact, there are two processes involved in this; gate control theory of pain and the descending inhibition.
Gate control theory of pain. This theory was coined in by two individuals by the name Melzack and Wall in the year 1965. According to Smeltzer et-al, "This theory proposed that stimulation of the skin evokes nervous impulses that are then transmitted by three systems located in the spinal cord. The substantia gelatinosa in the dorsal horn, the dorsal column fibres, and the central transmission cells act to influence nociceptive impulses".32 This theory postulated that there is a gated system that controls harmful signals.32 In this system, the gateway is unlocked when the thick threads are aroused and subsequently shut when the lesser strands in thickness are aroused.32 This system is controlled by electric signals originating from the cerebrum.32 This theory asserts that there are mental or emotional aspects participating in a critical role in the pain process. As a result, this theory has directed methodical investigations aimed at recognising and categorising psychosomatic and action based advances to the management of pain.32
Descending inhibition. The term descending inhibition denotes the dominant hindering pressures or control located on the nociceptors during the relay of signals to the cerebrum.33 According to Bountra, Munglani and Schmidt, there are a number of issues that lead to the stimulation of these pressures such as anxiety, trauma, dissemination and subsequent distribution of harmful signals, and tangential and other internal stimulus in the brain and spinal cord.34
Nociceptive pain. These are referred as pains that function and are subsequently controlled by the internal body tissues as opposed to tangential systems.35 This kind of pain is also relayed by the afferent strands characterised by reduced thickness and it passes through the gate mechanism coined in by Melzack and Wall (As elucidated earlier). Nociceptive pain is followed by swelling of body tissues, softness of the tissues, and an increase in temperature.35 In assessing this kind of pain, psychotherapist examines and investigates vigorousness in relation to mobility of the affected part of the body. Through this, s/he is able to identify and classify the kind of injury to the tissues. In other words, s/he is able to distinguish whether the injury has affected tangential or internal body tissues.36 Psychotherapists have adapted various techniques such as exercising the injured or affected part of the body, as well as habituating the swollen part.36 High temperatures, low temperatures, as well as ultrasound are used in the treatment of Nociceptive pain.
Figure 7: Transmission of Nociceptive pain.36
Source: Internet
Central sensitisation. This term is used to refer to the increase and augmentation of the role or function of neurons in the nociceptive courses or conduits.37 The augmentation is as a result of an elevation of the stimulation of outer surfaces of a cell or tissue, and as a result of minimised stimulation of the brain and spinal cord.37 This increase is what leads to swelling on the injured or damaged tissue.37 Olesen outlines some of the symptoms of central sensitisation to include elevated levels of sensitivity from illumination, contact, sound, chemicals, external strain, and temperature fluctuations.38 Treatment include relaxation, employment of electrical stimulants, channelled, psychological, or motor imagery, mirror psychoanalysis, and physical rehabilitation.38
Figure 8: The role of central sensitization.39
Neurogenic pain. Neurogenic pain is an immediate pain resulting from a cut, wound, or an ailments.35 According to Kumar and Saha, the main symptom of Neurogenic pain include "Reproduction of a patients pain during neurodynamic testing and presence of mechanical allodynia on nerve trunk palpation".35 Massaging the affected nerves or tissues is one of the treatment techniques used in treating this kind of pain.40 Additional treatment techniques include electrical stimulation of the nerves.40
Neurogenic/Neuropathic pain may occur at different parts of the body ranging from the nerve endings on the tangential sections to the cerebrum. Symptoms of this form of pain present themselves singly or may occur together. The symptoms include absence of feelings or consciousness, degeneration and total weakness of the muscles, pain on the skin as a result of touch, temporary itching or tingling sensation, and increased sensitivity to pain when exposed to heat. In assessing neurogenic pain, the initial phase is acquire the history of the painful occurrence. In taking the history, a physician focuses on the pattern, greatness, and length of the pain. There are various tools used in assessing this kind of pain. According to Bennett, these comprise of "neuropathic pain scale, leeds asssessment of neuropathic symptoms and signs (LANSS), neuropathic pain questionnaire, ID-pain and the Douleur neuropathique".41
Figure 9: Neurogenic pain.40
Case study: Trapped nerve at the back
John, a 30 years old man went to see his doctor complaining of incessant back pains developed after a lifting a heavy load.. This man had never undergone any surgery prior to the accident. His intention was to receive painkillers to relieve the pain.
Physical examination:
Height-------------------------5 ft 9 in
weight ----------------------------198 lb
Blood pressure-----------------132/89 mm Hg
Current Medication
Diazepam 10 mg 3 times a day
Assessment tools
Leeds Assessment of Neuropathic symptoms and Signs (LANSS) Questionnaire
Pain Detect Questionnaire
Tests
CT scan (computerised tomography)---------Showed a trapped nerve
Clinical representation
Lack of sensation
degeneration and total weakness of the muscles,
pain on the skin as a result of touch,
temporary itching or tingling sensation,
increased sensitivity to pain when exposed to heat
Treatment
Bed rest for two weeks
Regular massage
Apply ice and heat
Medication
Non-Steroidal anti inflammatory drugs (NSAIDs): Main objective to decrease puffiness or inflammation
Summary of the case study
In assessing his condition in order to identify the kind what was wrong, the doctor had to conduct physical examinations. After observation, the doctor inquired whether John had ever had any prior surgical procedure conducted on his back, to which he rebuffed. John explained to his doctor that he had difficulties performing his daily chores as the result of the back pain. In addition, John reported of poor coordination of his muscles especially the arms. His other reported signs included numbness, involuntary muscle movements, and a sharp pain on his lower back. The doctor had to conduct a CT scan (computerised tomography) to identify the extent of the damage. The doctor suspended a trapped nerve and his assumption was proven right by the CT scan.12 The diagram below from the Riverside Health Systems shows how a nerve may be trapped at the back.42
Figure 10: Trapped nerve42
In treating this condition, the doctor allotted Join painkillers to reduce the pain. In treating the involuntary muscle movements, the doctor gave John tablets known as diazepam whose main work is to relax the muscles. Subsequently, the doctor advised John to take as much rest as possible in a bid to try and avoid additional injury to the back. The doctor also recommended frequent back massages. For long term care, the doctor advised John to undergo physiotherapy.43
Conclusion
In conclusion, pain is considered a distasteful feeling that takes place immediately body tissues are injured or when the body is attacked by an ailment. The prevalence of pain is dependent on a number of factors including age, gender, level of income, occupation, and race or ethnicity. There are two major types of pain. These include acute and chronic pain. These are further divided into Nocigenic, Behavioural, Neurogenic, and psychogenic. Subsequently, pain is classified on the basis of its length, greatness, means, and according to medical perspective and situation. The pain pathway includes Nociceptors, and primary and secondary afferent fibres. Other forms of pain include Nociceptive pain, Central sensitisation, and Neurogenic pain. The Gate Control Theory of pain asserts that there is a gated system that controls harmful signals from being sent into the nervous system for processing. All the types of pain display have divergent characteristic in terms of their signs and symptoms, clinical representation, assessment, and the kind or types of assessment tools used.
References
1. Sofaer B. Pain: Principles, Practice and Patients. Cheltenham: Nelson Thornes, 2003. Print.
2. Stewart W F. The Epidemiology of Chronic Pain. Geisinger Center for Health Research. PowerPoint. n.d. 12 March 2014. < http://www.fda.gov/downloads/Drugs/NewsEvents/UCM307835.pdf >
3. Simpson D, McArthur J, Dworkin R. Neuropathic Pain: Mechanisms, Diagnosis and Treatment. New York: Oxford University Press, 2012: 90. Print.
4. Fishman S, Ballantyne J, Rathmell J. Bonicas Management of Pain. New York: Lippincott Wilkins & Wilkins, 2010: 699-790. Print.
5. Hecke O, Torrance N, Smith B. Chronic pain epidemiology-where do lifestyle factors fit in?." British Journal of Pain. 8.1 (2014): A4. JSTOR. Web. 12 Mar. 2014.
6. Haneline M, Meeker W. Introduction to Public Health for Chiropractors. London: Jones and Bartlett Publishers, 2011: 242. Print.
7. Schultz I, Gatchel R. Handbook of Complex Occupational Disability Claims: Early Risk Identification, Intervention, and Prevention. New York: Springer. 2005: 153. Print.
8. Marcus D. Chronic Pain: A Primary Care Guide to Practical Management. Pittsburgh: University of Pittsburgh, 2009. Print.
9. Yang J C, Tsui S L. A Guide to Pain Medicine. Hong Kong: Hong Kong University Press, 2002: 145. Print.
10. Shavizky A. Tackling the Measurability Problem of Physical Pain in Personal Injury Cases: The Case for Redeemed Pain and for Disregarding Race and Gender. Urbana: University of Illinois, 2008. Print.
11. "In the Face of Pain: Race and Pain." inthefaceofpain.com. Purdue Pharma, 2013. Web. 12 Mar 2014.
12. Murinson B. Take Back Your Back: Everything You Need to Know to Effectively Reverse and Manage your Back. Beverly: Fair Winds, 2011:34. Print.
13. Cousins M, Bridenbaughs. Neural Blockade in Clinical Anesthesia and Pain Medicine. New York: Lippincott Wilkins & Wilkins, 2012: 804. Print.
14. Finestone H. The Pain Detective: Every Ache Tells a Story. Santa Barbara: ABC- CLIO, 2009. Print.
15. Holdcroft A, Jaggar S. Core Topics in Pain. Cambridge: Cambridge University Press, 2005. Print.
16. Hardy P A, Hardy P A J. Chronic Pain Management: The Essentials. London: Greenwich Medical Media, 1997. Print.
17. Melnikova I. Pain classification and representative indications. Nature Reviews Drug Discovery 9.1 (2010): 589-590. Nature reviews. Web. 12 March 2014.
18. Bono J, eds. Revision Total Hip Arthroplasty. New York: Springer, 1999. Print.
19. Kaye A D, Urman R, eds. Understanding Pain: What you Need to Know to Take Control. Santa Barbara: ABC-CLIO, 2011. Print.
20. Clark G T, Dionne R A, eds. Orofacial Pain: A Guide to Medications and Management. Chichester: John Wiley & Sons, 2012. Print.
21. "New Directions to Improved Patient Care: Tutorial Series & Cases." A Pharmacists Roadmap to Pain Management. University of Kentucky., 2014. Web. 12 March. 2014.
22. Sinatra R, Jahr J, Watkins-Pitchford M. The Essence of Analgesia and Analgesics. New York: Cambridge University Press, 2011:3. Print.
23. Weiner R, eds. Pain Management: A Practical Guide for Clinicians, Sixth Edition. Boca Raton: CRC Press, 2002. Print.
24. Fishman S. Bonicas Management of Pain. New York: Lippincott & Wilkins, 2012: 1633. Print.
25. Glidden R, eds. Anesthesiology. Philadelphia: Lippincott and Wilkins, 2003:166. Print.
26. Webster R, eds. Neurotransmitters, Drugs and Brain Function. Chichester: John Wiley & Sons, 2001:177, 455. Print.
27. Snell R. Clinical Neuroanatomy. Philadelphia: Lippincott Williams and Wilkins, 2010: 143. Print.
28. Morris J S. Introduction to Data Modeling and Data Access Methods. Scientific Software Development. PowerPoint. 2013. 13 Mar 2014. < http://www.cgl.ucsf.edu/Outreach/bmi219/slides/data_modeling.html>
29. Moller A, ed. Reprogramming the Brain. Amsterdam: Elsevier, 2006:343. Print.
30. Freudenrich C. How Pain Works. (n.d). < http://science.howstuffworks.com/life/inside-the-mind/human-brain/pain.htm>
31. Robinson A. Clinical Electrophysiology: Electrotherapy and Electrophysiologic Testing. Philadelphia: Lippincott Williams & Wilkins, 2008:127. Print.
32. Smeltzer S O, Bare I, Hinkle J, Cheever K, eds. Brunner & Suddarths Textbook of Medical-surgical Nursing, Volume 1. Bellevue: Wolters Kluwer Health, 2010:235. Print.
33. Bodnar R, Commons K G, Pfaff D. Central Neural States Relating Sex and Pain. Baltimore: The John Hopkins University Press, 2002:157. Print.
34. Bountra C, Munglani R, Schmidt V, eds. Pain: Current Understanding, Emerging Therapies, and Novel Approaches to Drug Discovery. Cambridge: University of Cambridge, 2005:20. Print.
35. Kumar S, Saha S. Mechanism-Based Classification of Pain for Physical Therapy Management in Palliative care: A Clinical Commentary. Indian Journal of Palliative Care 17.1 (2011): 80-86. Print.
36. Tavares I, Martins I. Gene Therapy for Chronic Pain Management. Intech.2013. Web. 13 Mar. 2014. < http://www.intechopen.com/books/gene-therapy-tools-and- potential-applications/gene-therapy-for-chronic-pain-management >
37. Golan D, ed. Principles of Pharmacology: The Pathophysiological Basis of Drug Therapy. Baltimore: Lippincott Williams & Wilkins, 2008:271. Print.
38. Olesen J, ed. The Headaches. Philadelphia: Lippincott Williams & Wilkins, 2006:121. Print.
39. Massey A. Fibromyalgia. East Alabama Arthritis Center. 2014. Web. 13 Mar. 2014.
40. "Neuropathic Pain." EMed. Handbook Emergency Medicine Cork. 04 Sep 2010. Web. 13 Mar. 2014. < http://www.emed.ie/Analgesia/Pain_Neuropathic.php>
41. Bennett M. Assessment of neuropathic pain. Oxford Journals 8.6 (2008): 210-213.
42. Pinched Nerve. Riverside Health Systems. 2011. Web. 13 Mar. 2014. < http://www.riversideonline.com/health_reference/Nervous- System/DS00879.cfm?RenderForPrint=1>
43. Barazer A. Trapped Nerve in Back: How to Treat and Prevent this Painful Condition. Energy Medicine Clinic. 20 October 2013. Web. 13 Mar. 2014. < http://www.energymedicineclinic.co.uk/trapped-nerve-in-back/#>
Read
More
CHECK THESE SAMPLES OF The Neurophysiology of Peripheral Neurogenic Pain
Alternative Pain Management
From the paper "Alternative pain Management", understanding the mechanism of pain and devising strategies for pain management has been the goal of researchers for centuries.... In some situations, excruciating pain is borne without a twinge, while in others a mild pain can be unbearable.... International Association for the Study of pain defines pain as 'an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage' (Chen, 2004)....
6 Pages
(1500 words)
Essay
Peripheral Intravenous Therapy
This paper "Peripheral Intravenous Therapy" is about changing the management of peripheral intravenous therapy in an intermediate rehabilitation ward.... peripheral Intravenous Therapy refers to the injection of liquid substances directly into a vein of the arm, hand, leg, foot, and scalp which can be intermittent or continuous.... A peripheral IV line consists of a short catheter (a few centimeters long) inserted through the skin into a peripheral vein....
13 Pages
(3250 words)
Essay
Neurophysiology of Sleep
The essay "Neurophysiology of Sleep" focuses on the critical analysis of the major disputable issues concerning the neurophysiology of sleep.... It is thought that for cerebral representations to be modified or updated, the cells over the whole cerebral cortex should become modifiable....
5 Pages
(1250 words)
Essay
Peripheral Arterial Disease (PAD)
One of the main symptoms in a person with PAD is intermittent claudication, 'which is pain or weakness with walking that is relieved with rest' (Aronow 2007).... Most commonly, atherosclerosis affects the superficial femoral and popliteal arteries, and thus, the pain is most often in the calf muscle.... In case the atherosclerotic obstruction is at the distal aorta and its bifurcation into the two iliac arteries, the pain may be felt, in addition to the calf, in the buttocks, hips, thighs, or the inferior back muscles (Aronow 2007)'The Rutherford classification of PAD includes 7 stages....
12 Pages
(3000 words)
Essay
Peripheral arterial disease (PAD)
his is the clinical history of a 70-year old man who presented in the hospital with symptoms of pain in the calf muscle with walking that was relieved with rest.... peripheral arterial disease (PAD) is a chronic arterial occlusive disease of the lower extremities as result of atherosclerosis.... Earlier, CTA technology was able to image only a portion of the peripheral arterial tree.... Thus, the multi-detector row CT angiography (MDCTA) has developed as an accurate method in assessing the peripheral arteries....
11 Pages
(2750 words)
Essay
The Possible Pathophysiological Mechanism behind Chronic Regional Pain Syndrome
The author of this coursework "The Possible Pathophysiological Mechanism behind Chronic Regional pain Syndrome" describes the CRPS disorder.... The main symptom representing this disease is intense pain, out of proportion to the level of injury, which goes on worsening rather than getting better with time.... Treatment for chronic regional pain syndrome is most effective when started early in the course of the syndrome.... The soldiers noted burning pain, progressive skin changes, and decreased function in an affected limb....
14 Pages
(3500 words)
Coursework
The Relationship of Chiropractic With Biology
This research paper "The Relationship of Chiropractic With Biology" examines how chiropractic relates to the field of biology.... While biology encompasses knowledge of the living matter, it presents only facts, the laws of which are related to nature whether in health or disease.... .... ... ... This paper investigates how chiropractic is related to biology....
11 Pages
(2750 words)
Research Paper
Situated Learning Theory; Legitimate Peripheral Participation
The author of the paper "Situated Learning Theory; Legitimate peripheral Participation" notes that the two scholars Lave J.... The theory has been stated by many scholars over a period including others who have argued in its favor after Lave and Wenger came up with the 'legitimate peripheral participation' theory of the situated learning theory.... he theory of situated learning; legitimate peripheral participation, argues that learning takes place through what is referred to as communities of practice....
59 Pages
(14750 words)
Literature review
sponsored ads
Save Your Time for More Important Things
Let us write or edit the essay on your topic
"The Neurophysiology of Peripheral Neurogenic Pain"
with a personal 20% discount.
GRAB THE BEST PAPER

✕
- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY