StudentShare


Our website is a unique platform where students can share their papers in a matter of giving an example of the work to be done. If you find papers
matching your topic, you may use them only as an example of work. This is 100% legal. You may not submit downloaded papers as your own, that is cheating. Also you
should remember, that this work was alredy submitted once by a student who originally wrote it.
Login
Create an Account
The service is 100% legal
- Home
- Free Samples
- Premium Essays
- Editing Services
- Extra Tools
- Essay Writing Help
- About Us
✕
- Studentshare
- Subjects
- Nursing
- Hand Hygiene and Infection Control
Free
Hand Hygiene and Infection Control - Literature review Example
Summary
"Hand Hygiene and Infection Control" paper analizes five studies in the field of hand hygiene and its usage in preventing infections within hospital settings. These studies are selected from A-rated databases such as Ebscohost, Science Direct, and Emerald Insight. …
Download full paper File format: .doc, available for editing
GRAB THE BEST PAPER98% of users find it useful
- Subject: Nursing
- Type: Literature review
- Level: Undergraduate
- Pages: 16 (4000 words)
- Downloads: 1
- Author: dpowlowski
Extract of sample "Hand Hygiene and Infection Control"
Hand Hygiene and Infection Control Hand Hygiene and Infection Control Introduction In the medical discipline of Epidemiology, there is a sub-discipline, which deals with controlling nosocomial or healthcare-related infections called infection control or infection prevention. Despite the fact that epidemiology is an underrated field of study in medical science much focus has been laid on formulating policies and measures that prevent infections to take place (Smith, 2009; Oittet, 2008). Therefore, it can be asserted that infection prevention measures holds pivotal importance for a hospital’s management, which can be achieved by establishing concrete health-care delivery mechanisms. Infection control measures include a number of sub-fields such as use sterilized hospital equipment, hand hygiene and etc. (Takahashi & Turale, 2010; Penzias, 2010). Keeping this in view, the author of the current research paper would focus on discussing infection control measures with respect to its success by implementing hand hygiene matters. For this reason, the author has selected five studies in the field of hand hygiene and its usage in preventing infections within hospital settings. These studies are selected from A-rated databases such as Ebscohost, Science Direct and Emerald Insight. By the end of this research paper, readers would be able to understand how maintaining hand hygiene helps nursing staff and hospital management to prevent infections to occur.
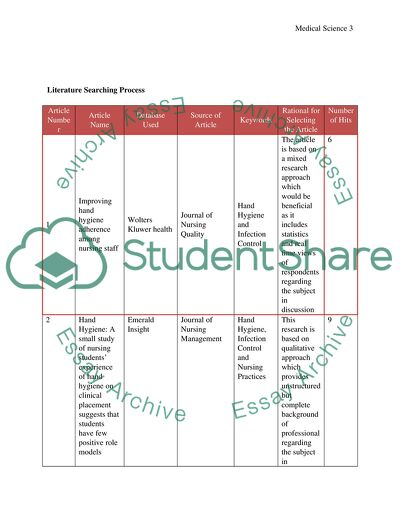
Literature Searching Process
Article Number
Article Name
Database Used
Source of Article
Keywords
Rational for Selecting the Article
Number of Hits
1
Improving hand hygiene adherence among nursing staff
Wolters Kluwer health
Journal of Nursing Quality
Hand Hygiene and Infection Control
The article is based on a mixed research approach which would be beneficial as it includes statistics and real time views of respondents regarding the subject in discussion
6
2
Hand Hygiene: A small study of nursing students’ experience of hand hygiene on clinical placement suggests that students have few positive role models
Emerald Insight
Journal of Nursing Management
Hand Hygiene, Infection Control and Nursing Practices
This research is based on qualitative approach which provides unstructured but complete background of professional regarding the subject in discussion
9
3
A systematic review of hand hygiene improvement strategies: a behavioral approach
Emerald Insight
Journal of Implementation Science
Infection Prevention, Medical Procedures, Nursing Staff
The article is based on a mixed research approach which would be beneficial as it includes statistics and real time views of respondents regarding the subject in discussion
11
4
The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including hand washing and alcohol-based hand sanitizers
Science Direct
American Journal of Infection Control
Healthcare safety measures, infection control and hand hygiene
The article is based on a mixed research approach which would be beneficial as it includes statistics and real time views of respondents regarding the subject in discussion
58
5
Effect of Hand Hygiene on Infectious Disease Risk in the Community Setting: A Meta Analysis
National Center for Biotechnology Information
American Journal of Public Health
Infection control, Hand Hygiene and Nursing
The article is based on a mixed research approach which would be beneficial as it includes statistics and real time views of respondents regarding the subject in discussion
165
Research Considerations
A research based on qualitative methodology would consist of findings retrieved from qualitative data such as in-depth analysis of previously published literature, interviews with the sample and formulating results based on identified themes. On the other hand, a quantitative research study would be based on quantified results, and the findings will be formulated based on statistical information retrieved from the primary research. For a research work, data can be collected by various means such as interviews, surveys or focus group discussion with the identified sample. Moreover, previously published literature on the same subject will also be helpful in data collection. While carrying out a research work, the researcher must comply with certain ethical considerations. First of all, he/she should ensure that information provided by respondents should not be leaked or sold out to any third party. Moreover, it is the moral responsibility of the researcher to ensure that he/she should not commit plagiarism of others’ ideas and findings.
Literature Review
Infection Control
Infection prevention measures refer to a healthcare setting’s actions against the spread of infections and disease control. It is not necessary that the infection control measures are aimed at reducing the chances for infection take place by infusion or transfer of objects from patient-to-patient, but it also includes reducing the chances of infection to occur by exchange of an object from patient-to-staff, staff-to-patient or staff-to-staff. Infection controlling measures are implemented to different functions of nursing staff such as their hand Hygiene, hand and equipment cleaning, disinfection, sterilization, vaccination or surveillance and etc. (Centers for Disease Control and Prevention, 2013). Infection control measures are also required to be adopted during diagnosis, monitoring of the patients or assessing the chances for an infection to spread within the healthcare setting. In this manner, Infection Prevention and Control is the academic terminology, which is used for this field (Smith, 2009).
It is evident from the available literature on infection control that healthcare workers are highly exposed to different cadres of infections while performing their respective duties. More importantly, nursing staff is the one who is responsible to take care of patient round the clock (Harne-Britner et al., 2011). During their 8 hour long shift at the hospital, nursing staff not only take care of medication and dietary plan of the patients, but also perform the duty of preventing infections to occur. In this manner, they are exposed to infections throughout the span of their job at the healthcare setting. For this reason, different vaccinations are available in the market, which helps nursing staff to avoid infections to affect them (Seao, 2011). Hospitals adopt different regulations and legal frameworks to urge nurses to comply with the hygiene and infection control systems of the organization. In the same manner, patients are also provided with different vaccinations to avoid the hazardous impact of different infections prevailing in a healthcare setting (Maskerine & Loeb, 2006; Duffin, 2008). Both patients and nursing staff is provided with vaccines that help them to fight against Hepatitis B, Measles, Rubella, Influenza, mumps, Tetanus, Diarrhea and etc. Although vaccines are quite effective in providing patients and hospital staff with protection against different infections, they do not guarantee the prevention completely and possess some adverse reverse effects (Ott & French, 2009).
To manage a situation in which infections occur more frequently in a healthcare setting, hospitals adopt different procedures and systems through which the effect of infection can be minimized or completely avoided (Curry & Cole, 2005). Standard infection prevention and controlling system, which is practiced globally, are discussed in the lines below:
1. Surveillance for Preventing Infections: Surveillance for the sake of monitoring the situation of infection prevalence in a health care setting is an effective practice. By conducting surveillance in the infection-hit area in a hospital setting, the hospital staff is able to identify the presence of infection by going through the patient charts and nursing staff’s health report. During this activity, hospital’s patients and nursing staff is scrutinized for the presence of any signs or symptoms of an infection. The focus of infection control practitioner is identifying the presence of infection in the bloodstream, urinary tract, surgical equipment and other instruments which are used by nursing staff on the patients and may catch infected germs and microbiological elements. To carry out surveillance, hospitals’ infection control practitioners make use of quantitative data in order to keep an eye on the numbers and statistics related to infection’s presence in the hospital environment (Boyce, 2008). By doing so, hospital staff could make suitable arrangements in advance to totally avoid the infection to occur or reduce its adverse effects by proposing strategies or medical plans for the hospital staff and patients. Moreover, computer software is also readily available in the market, which helps the hospital management to identify potential threat to infection control mechanism of the organization. It is estimated that infection surveillance mechanisms of hospitals in United States reduce the rate of infection occurrence by 32% annually (Momen & Fernie, 2010).
2. Outbreak Investigation: This is a post-infection occurrence procedure, which helps in identifying possible remedies to the infection. Upon identifying regular illness among nursing staff or deteriorating conditions of the patients, hospital’s infection prevention practitioners carry out the outbreak investigation to identify the type of infection, its reasons to occur, person who is responsible to spread the infection and the possible vaccination or remedies that are available in the market (Motacki & Kapoian, 2011). The outbreak investigation also helps hospital’s management to categorize the infection outbreak. Such as, a pseudo-infection outbreak, which is usually, a wrong alarm, infection causing random irregularities in the health chart of nursing staff or the patients and a true infection outbreak. Upon identifying the occurrence of infection within the healthcare setting, the infection prevention practitioners of the hospital would first identify the reasons or breach of healthcare policy that allowed the infection to occur and how the infection can be prevented to spread to other patients and nursing staff (Fraise et al., 2012). As outbreak investigation of infections is a post-occurrence practice, therefore it is helpful in reducing the effects of already occurred infection, stopping it to spread to other patients and staff, identifying strategies to avoid the infection in the future and learn how the infection would lead to the occurrence of other infections within the healthcare settings (Maxfield & Dull, 2011).
3. Training and Development of Nursing Staff: Another important responsibility of infection prevention practitioners in a healthcare setting is to train employees regarding the strategies to avoid infections to occur or reducing the adverse effects of an infection that already occurred. For this reasons, hospitals acquire the service of specialized infection prevention practitioners who are responsible to train nursing staff about how they can protect themselves and patients from getting infected, how preliminary measures can reduce the chance of infection outbreak or how they should act in case an infection already occurred (Elsevier Health Sciences, 2008). For this reason, organizations provide their employees with facilities to acquire certificates and awards upon completing infection control and prevention practitioner courses to support its employees’ actions against infections (Mani et al., 2010).
This section helped the readers to create understanding of different infections that might outbreak in a healthcare setting, how to avoid these infections and how to reduce the adverse effects of infection. In this discussion, hand Hygiene had been identified as the main source of generating or spreading infections in the healthcare setting. In this regard, the focus of the paper would be laid on hand hygiene in the next section.
Hand Hygiene
Nursing staff of a healthcare setting is the one whose hands come into close contact with the patients while carrying out a diagnosis or their daily patient care. This might include hand contact with the patient while contacting contaminated surfaces, or placing and shifting a device or materials such as changing the dress of the patient. In this scenario, it is eminent that the patient or the nursing staff might catch infections, which highlights the importance of hand Hygiene in a healthcare setting (Joint Commission Resources, 2008). In the modern healthcare environment, hand Hygiene has its importance in the heart of the medical procedures as it provides a cheap and easily adoptable strategy to reduce the chances of infection breakout within the hospital. Hand Hygiene procedures are developed and implemented in a way that they help the nursing staff to save precious lives and deliver a protected treatment to patients (Kampf & Loffler, 2010).
Hand Hygiene is also referred to as hand antisepsis, hand degerming, hand decontamination, and hand sanitizing or hand disinfection. But the essential theme that is identified in the literature pertaining to hand Hygiene denotes it as an act of washing hand with antibacterial soap or sanitizer (Bowden & Greenberg, 2011). Majority of the time, hand sanitizing is carried out with alcoholic hand soap or rubs which helps the user to remove any dirt or microbial element on the surface of their skin (Davnani et al., 2011).
As the nursing staff of a hospital is present at the healthcare setting for 24 hours a day and 7 days a week, it is important for them to adopt the habit of sanitizing their hands before and after carrying out a diagnose, changing patients clothes and serving them medication. It is clear that the nursing staff plays an important role in a hospital’s functional capacity therefore, it is of pivotal importance for the nursing staff to comply with the hand Hygiene policies. Keeping hand Hygiene’s importance in health service delivery, countries have adopted multiple policies and regulations that require nurses to keep their hands protected to reduce the chances of any infection outbreak (Basford & Slevin, 2003). For example in UK, Nursing and Midwifery Council (NMC) urges its associates and member nursing staff to protect their patients from any infection outbreak. Similarly, in USA there are a number of strategies, regulations and policy frameworks that prohibit from making a contact with patients or providing them with medication and equipment before taking care of their hand hygiene (Canham, 2011).
Despite of number literatures highlighting the importance of hand hygiene in a healthcare setting, there are still evidences of low compliance with hand Hygiene policies and regulations within a healthcare setting. The major reason identified for non-compliance with the hand Hygiene policies is that, nurses perceive it is the utter responsibility of infection control practitioners to prevent infection breakout (Koutoukidis et al., 2012). Other reasons for non-compliance of hand hygiene policies are that, nurses have a hectic schedule during their shifts, whereas taking care of hand Hygiene is a time consuming task that collides with their daily routine tasks. On the other hand, presence of accessories like gloves as an alternative infection control measure also prevents nurses to adopt hand Hygiene measures. But researches show that even after using gloves, there are chances that infection breakout will occur. This is because; most of the time nurses do not prefer to wash or sanitize their hands after removing the gloves and move on to other patient for their diagnosis or medication supply (Sitzman & Eichelberger, 2004). Another major reason for nurses not sanitizing their hands is that, nurses perceive hand sanitizers or hygiene would cause allergy or problems for their skin. These kinds of perceptions are usually associated with the use of alcoholic hand rubs, which nurses perceived as being harmful for their skin (Cambell, 2010). Ott et al. (2009) suggests, “The attitudes and behavior towards hand hygiene is a complex issue, involving the perception of its effectiveness, staff’s values and beliefs and existing barriers. In order to achieve high compliance rates with hand hygiene, the defaulters should be disciplined as though they have violated hospital policy, starting with personal counseling to verbal warning and eventually to a written warning placed in their file” (Ott & French, 2009).
Considering Otte et al. (2009)’s assertion pertaining to hand Hygiene, it can be inferred here that hand Hygiene is not solely the responsibility or problem of the hospital staff. It should be considered as the shared responsibility of hospital’s management, physicians, nursing staff, administrating staff, patients and janitorial staff to keep their hands clean in order to prevent breakout of infections. Collins et al. (2005) suggests that patients have an important role to play to ensure compliance with hand hygiene policies and regulations. This is because; patients are the one who are most affected by the infections caused by bad hand Hygiene. In this respect, they should ask the attending physician or nursing staff if they have taken care of their hand hygiene. If the patient identifies that the source of his or her illness or infection outbreak belongs to the hospital or its staff, the he or she can sue the hospital for non-compliance with the hand Hygiene regulations and frameworks. On the contrary, the hospital staff should not create a situation where the organization will have to face embarrassment because of legal actions taken by the customer as the patients consider as a betrayal of trust if they are not provided with standardized medical procedures (Daly et al., 2009).
The question, which arises here, is that what are the effective techniques to keep the hospital staff’s hand hygienic. There are a number of techniques, which might be useful in preventing infections caused bad hand hygienic conditions. The primary responsibility of the nursing staff before and after making contact with the patient is that, they should remove any visible soil particles or remaining of microbial elements from their skin. Besides, there are several pathogens available to healthcare practitioners, which are beneficial for removing contaminated microbial particles from hands. Another source of infection outbreak could be transient flora, which is caused by routine checkup of the patients (Craven & Hirnle, 2007). Transient flora can also be present in the hospital’s environment, furniture fixings, and medical equipment. These can be easily avoided by certain mechanical procedures such as producing friction by rubbing your hands tightly while washing (Akyol, 2007).
A number of antimicrobial soaps and hand rubs with alcohol in it are also available in the market. These sanitizers are beneficial for reducing the risk of cross infection caused during examining a patient. Effective hand washing techniques can also prove to be beneficial in reducing the chances of any infection occurring within the healthcare setting (Kozier, 2008). Akyol (2007) states, “Effective hand washing is the application of a plain (non-antimicrobial) or antiseptic (antimicrobial) soap onto wet hands; then vigorous rubbing together of both hands to form a lather, covering all the surface of the palms, tops of the hands, base of the fingers, between the fingers, back of the fingers, fingers tips, fingernails, thumb and wrists for one minute” (Akyol, 2007). Other techniques, which will prove to be beneficial in controlling infection outbreak, can be:
Nursing staff and physicians should keep their fingernails short
Artificial finger nails should be avoided as they contain microbial components
Microbial load should be removed from the finger nails on a daily basis
Chipped nail polish brands should be avoided
Hand jewelry or wristwatches should be avoided as they may contain microbial elements in the skin underneath them
Nursing staff should rinse their hands completely after washing them
Important consideration should be paid towards removing lather after washing them with soap sanitizer
Hands should not be rinsed with hot water or tap water in order to avoid skin dryness (Kilpatrick et al., 2013).
It has been observed that hand drying also holds pivotal importance in keeping hands hygienic and infection free. This is because; microorganisms make their place in hands in damp surrounding which may generate microbial which causes infection to the patients. In order to use gloves before examining patients or providing them with medication, nursing staff should wash their hands and dry them by using a hot-air blower. Moreover, hands should be rubbed against each other so that organism from the palm can be removed. Moreover, nursing staff should also avoid touching the taps after cleaning their hands. Instead of using fabricated towels, nursing staff is recommended to use paper towels to rinse hands (Werner, 2007).
The discussion carried out in this section helped the readers to understand why hand Hygiene is important for preventing infections to occur and what are the techniques to avoid development of infections caused by bad hand hygiene. The next section would focus on presenting researches and studies carried out by medical practitioners and scholars in the past, pertaining to hand Hygiene and its relevance with infection control.
Infection Control and Hand Hygiene
Bloomfield et al. (2007) carried out a research work in order to identify how hand hygiene procedures can be beneficial in minimizing the risk of infections. The sub-topic of their research work was based on identifying the effectiveness of using hand washing and alcohol-based sanitizers for hand hygiene. For this purpose, the selected sample for their research work was selected from developed countries in North America and Europe, where the rate infection breakout because of hand hygiene is minimum. By using a mixed approach to research work, i.e. both quantitative and qualitative research approach, the researchers identified, “Hand hygiene is a key component of good hygiene practice in the home and community and can produce significant benefits in terms of reducing the incidence of infection, most particularly gastrointestinal infections but also respiratory tract and skin infections” (Bloomfield et al., 2007). Moreover, the researchers also inferred that decontaminating hands with soap or sanitizers that do not contain water particles would be beneficial for reducing the chances of infection breakout.
Aiello et al (2008) carried out a quantitative study to understand the effect of hand-hygiene interventions on probability of infections such as gastrointestinal and respiratory illnesses. To make the intervention, the researchers utilized a sample of 4 electronic databases to retrieve quantitative findings of researches carried out in the same area. The data was selected from January 1960 to May 2007 for carrying out the meta-analysis. The results retrieved from the meta-analysis helped the researchers to infer that hospitals and healthcare settings should continuously carry out community based hand hygiene activities to create awareness what medical practitioners, nursing staff and patients should do to avoid infection to occur. Moreover, the researchers presented a number of recommendations for future studies in the same field, which would be beneficial in identifying further techniques to prevent infections to occur from bad hand hygiene.
Huis et al. (2012) systematically reviewed the need for improvement in hand hygiene strategies keeping in view the behavioral aspects of human nature. The primary purpose of the study was to identify the basic reasons behind patients and nursing staff’s negligence towards complying with the hand hygiene protocols. In order to attain the desired objectives of the research study, the researchers used systematic search of literature available on hand hygiene. For this purpose, the researchers utilize a number of databases from January 2000 to November 2009. The first step that researchers took was to study salient features of hand hygiene compliance using the EPOC Data Collection Checklist. The last step to complete the research work was to use the Taxonomy of Behavioral Change Techniques in order to identify the determinants. The findings of Huis et al (2012)’s research suggests that lack of awareness, action control, lack of knowledge about infection that might break by bad hand hygiene and facilitation trend of nursing staff and patient’s behavior are the cause of infections caused by bad hand hygiene.
Birtner (2011) carried out a study to explore the initial and sustained effects of educational and behavioral interventions on hand hygiene. In particular, the research area focused on adherence of hand hygiene regulations and link between cross infection occurrence and hand hygiene regulation adherence. The researchers adopted a quantitative approach of research work and a quasi-experimental model was implemented. The sample for the research work consisted of nursing staff from 3 units in a hospital, and they were divided into two experimental and one control group. The control group was provided with educational material pertaining to hand hygiene whereas, the experimental groups were provided with behavioral interventions in support with educational material. The study outcomes suggested that no difference is observed in the rate of infection occurrence found in the nursing groups; let it be controlled or experimental group. Moreover, it was also found that nursing staff belonging to both groups does not show any difference with regards to their adherence to the hand hygiene regulations.
Lusardi (2007) carried out a study in the field of nursing, which focused on understanding the student nurses’ experience of hand hygiene on clinical placement. For this purpose, researcher selected a sample of nine nurse student volunteers and interviews with these volunteers were conducted. The basic themes identified as a result of interviews pertaining to student nurses’ perspective and experience of hand hygiene in a clinical practice was as following:
Responsibility: It is the responsibility of patients and nursing staff to maintain hand hygiene and prevent related infections.
Influences: Senior-nursing staff should play the role model and adopt hand hygiene practices that could be followed by the junior nursing staff.
Reasons for poor nursing practice: Complacency and wrong perceptions related with hand hygiene leads nursing staff towards not complying with the decontamination policies pertaining to hand hygiene.
Socialization: As a majority of nurses do not comply with hand hygiene decontamination policies and regulations, the nursing staff finds it unnecessary to comply with the regulation as well.
Conclusion
From the discussion carried out in this research paper regarding hand hygiene and infection prevention and control, the basis themes identified are as following:
Nursing staff is afraid of allergies and after effects of using sanitizers and soaps.
Nursing staff could not get enough time during their shifts to decontaminate hands.
Nursing staff follows their seniors, who are reluctant towards using decontamination procedures.
If fellow nursing staff does not comply with the hand hygiene regulations, then other nurses would also do the same.
Absence of training, development and education among nursing staff and patients pertaining to hand hygiene are the biggest cause of infections caused by bad hand hygiene.
From the analysis of reviewed literature, educating and creating awareness about the harmful effects of bad hand hygiene habits, is identified as the best alternative approach available to medical practitioners. By educating their nursing staff and patients, it would become easier for the healthcare institutions to prevent and control the outbreak of infections.
List of References
Aiello, E, A., Coulborn, R.M. & Larson, E.L., 2008. Effects of Hand Hygiene on Infectious Disease Risk in the Community Setting: A Meta-Analysis. American Journal of Public Health, 98(8), pp.1372-81.
Akyol, A.D., 2007. Hand hygiene among nurses in Turkey: opinions and practices. Journal of Clinical Nursing, 16, pp.431-37.
Basford, L. & Slevin, O., 2003. Theory and Practice of Nursing: An Integrated Approach to Caring Practice. NY: Nelson, Thornes.
Bloomfield, S.F. et al., 2007. The effectiveness of hand hygiene procedures in reducing the risks of infections in home and community settings including handwashing and alcohol-based hand sanitizers. American Journal of Infection Control, 35(10), pp.27-64.
Bowden, V.R. & Greenberg, C.S., 2011. Pediatric Nursing Procedures. NY: Lippincott Williams & Wilkins.
Boyce, J., 2008. Hand hygiene compliance monitoring: Current perspectives from the USA.. Journal of Hospital Infection, 70, pp.2-7.
Cambell, R., 2010. Hand-washing compliance goes from 33% to 95% steering team of key players drives process. Healthcare Benchmarks and Quality Improvement , 17(1), pp.5-6.
Canham, L., 2011. The first step in infection control is hand hygiene. The Dental Assistant, pp.42-46.
Centers for Disease Control and Prevention, 2013. Hand Hygiene Saves Lives. [Online] Available at: [Accessed 5 February 2014].
Collins, F. & Hampton, S., 2005. Hand-washing and methicillin-resistant staphylococcus aureus. British Journal of Nursing, 14(13), pp.703-07.
Craven, R.F. & Hirnle, C.J., 2007. Fundamentals of Nursing: Human Health and Function. NY: Lipincott Williams & Wilkins.
Curry, V. & Cole, M., 2005. Applying social behavioral theory as a template in contracting and confining VRE. Critical Care Nurse Quarterly, 24(2), pp.13-19.
Daly, J., Speedy, S. & Jackson, D., 2009. Contexts of Nursing. Sydney: Elsevier Australia.
Davnani, M., Kumar, R., Sharma, R.K. & Gupta, A.K., 2011. A survey of hand-washing facilities in the outpatient department of a tertiary care teaching hospital in India. Journal of Infection in Developing Countries, 5(2), pp.114-18.
Duffin, C., 2008. Leadership and workload key to infection control. Nursing Standard, 22(47), p.7.
Elsevier Health Sciences, 2008. Evidence-based Nursing Care Guidelines: Medical-surgical Interventions. NY: Elsevier Health Sciences.
Fraise, A., Maillard, J.-Y. & Sattar, S., 2012. Russell, Hugo and Ayliffes Principles and Practice of Disinfection, Preservation and Sterilization. NJ: John Wiley & Sons.
Harne-Britner, S., Allen, M. & Fowler, K.A., 2011. Improving hand hygiene adherence among nursing staff. Journal of Nursing Care Quality, 26(1), pp.39-48.
Huis, A. et al., 2012. A systematic review of hand hygiene improvement strategies: a behavioural approach. Implementation Science, 7(92), p.Online.
Joint Commission Resources, 2008. Hand Hygiene: Toolkit for Implementing the National Patient Safety Goal. NY: Joint Commission Resources.
Kampf, G. & Loffler, H., 2010. Hand disinfection in hospitals-benefits and risks. Journal of the German Society of Dermatology, 8(12), pp.978-83.
Kilpatrick, C., Hosie, L. & Storr, J., 2013. Hand hygiene – when and how should it be done? [Online] Available at: [Accessed 5 February 2014].
Koutoukidis, G., Stainton, K. & Hughson, J., 2012. Tabbners Nursing Care: Theory and Practice. NY: Elsevier Health Sciences.
Kozier, B., 2008. Fundamentals of Nursing: Concepts, Process and Practice. Ny: Pearson Education.
Lusardi, G., 2007. Hand Hygiene: A small study of nursing students experiences of hand hygiene on clinioal placement. Nursing Management, 14(6), pp.26-33.
Mani, A., Shubangi, A.M. & Saini, R., 2010. Hand hygiene among healthcare workers. Indian Journal of Dental Research, 21(1), pp.115-18.
Maskerine, C. & Loeb, M., 2006. Improving adherence to hand hygiene among health care workers.. Journal of Continuing Education in the Health Professions, 26(3), pp.244-51.
Maxfield, D. & Dull, D., 2011. Influencing hand hygiene at spectrum health. Physician Executive Journal , 37(3), pp.30-34.
Momen, K. & Fernie, G.R., 2010. Nursing activity recognition using an inexpensive game controller: an application to infection control. Journal of European Society for Engineering and Medicine, 18(6), pp.393-408.
Motacki, K. & Kapoian, T., 2011. An Illustrated Guide to Infection Control. NY: Springer.
Oittet, D., 2008. Hand hygiene: it’s all about when and how (commentary). Infection Control and Hospital Epidemiology, 29(10), pp.957-59.
Ott, M. & French, R., 2009. Hand hygiene compliance among healthcare staff and student nurses in a mental health setting. Mental Health Nursing, 30, pp.702-04.
Penzias, A., 2010. Don’t get complacent with hand hygiene. ED Nursing, 13(5), pp.54-55.
Sarah, H.-B., Marianne, A. & Kimberley, F., 2011. Improving Hand Hygiene Adherence Among Nursing Staff. Journal of Nursing Care Quality, 26(1), pp.39-48.
Seao, M.J., 2011. Hand Hygiene Compliance: A Multidisciplinary & Proactive Approach. [Online] Available at: [Accessed 5 February 2014].
Sitzman, K. & Eichelberger, L.W., 2004. Understanding the Work of Nurse Theorists: A Creative Beginning. California: Jones & Bartlett Learning.
Smith, S.M., 2009. A review of hand-washing techniques in primary care and community setting. Journal of Clinical Nursing, 18(6), pp.786-90.
Smith, S., 2009. A review of hand-washing techniques in primary care and community settings. Journal of Clinical Nursing, 18(6), pp.786-90.
Takahashi, I. & Turale, S., 2010. Evaluation of individual and facility factors that promote hand washing in aged-care facilities in Japan. Nursing and Health Sciences, 12(1), pp.127-34.
Werner, R., 2007. Hand washing and what happens if you don’t. Massage and Bodywork, 22(2), pp.114-18.
Read
More
CHECK THESE SAMPLES OF Hand Hygiene and Infection Control
Central Venous Catheter Infection Problem
An 18-month prospective, nested case-control study for 55 patients with bloodstream infection (BSI) and 55 without BSI shows an increased length of stay in ICU for patients with central venous catheter-associated BSI.... This paper "Central Venous Catheter infection Problem" is focused on the problem of CVC infection problem discussion.... This paper will present a literature overview of the theme related to the challenges of CVC infection problem and correlate it with the problem of nursing practices....
15 Pages
(3750 words)
Literature review
Infection Control and Hand Hygiene
This paper 'infection control and Hand Hygiene' discusses the infection control and hand hygiene.... The purpose of the research is to discuss various issues to help understand what infection control and hand hygiene is and how the two are related.... infection control looks to prevent those who might be in danger of acquiring deadly diseases and infections.... Secondary Research This is a qualitative research on the topic infection control and hand hygiene....
20 Pages
(5000 words)
Literature review
Hand Hygiene in infection control
Hand Hygiene in infection control Instructor Date Hand Hygiene in infection control The term hand hygiene describes the process of decontaminating hands through hand washing using either water with plain soap, antibacterial soap or by using alcohol based products that contain emollient (PAC and the HICPAC/SHEA/APIC/IDSA, 2002).... Hand Hygiene in infection control Hand Hygiene in infection control The term hand hygiene describes the process of decontaminating hands through hand washing using either water with plain soap, antibacterial soap or by using alcohol based products that contain emollient (PAC and the HICPAC/SHEA/APIC/IDSA, 2002)....
3 Pages
(750 words)
Essay
Evaluation of Infection Control in Hospitals
Through the years, more understanding of the connection between hygiene and infection was obtained that led to improvements in the hospital setting which was later coupled with the introduction of the use of antiseptics during surgery.... The essay "Evaluation of infection control in Hospitals" analyzes the major issues in the evaluation of infection control in hospitals.... The National Audit Office noted in its 2000 report that nine percent of all inpatients or one in every eleven inpatients in England had a hospital-acquired infection at any one time....
8 Pages
(2000 words)
Essay
Project Management: Hand Hygiene in Hospitals
"Project Management: Hand Hygiene in Hospitals" paper studies the importance of Hand Hygiene and Infection Control in the health care setting.... The main purpose of this project is to study and know the importance of Hand Hygiene and Infection Control in the health care setting.... In real life, the control of these dual systems is always quite diverse, and due to that needs the growth of specific technical experience and management techniques....
8 Pages
(2000 words)
Coursework
Project Management, Practice through the 4-D Model
It is highly important to sensitize adults to the need to wash their hands to control infections.... (2013), 70% of hygiene-related diseases are transferred through hand contact.... Fraise and Bradley (2009) emphasize the need for effective hand washing to prevent the transfer of germs through hand contact.... Hospital-acquired infections (HAIs) are typically associated with improper hand washing.... roper hand washing among patients and healthcare personnel is important in the prevention of HAIs....
8 Pages
(2000 words)
Research Paper
The Effects Associated with Poor Hand Hygiene by Healthcare
"The Effects Associated with Poor hand hygiene by Healthcare" paper provides insight in order to ensure that the HAIs are given adequate attention.... This research proposal is an endeavor to elucidate the effects associated with poor hand hygiene by healthcare providers in an attempt to establish a strategy for the prevention of HAI.... The Centre for Disease control (CDC, 2014) has reported approximately two million patients fall victim to HAI annually and over 100,000 deaths....
11 Pages
(2750 words)
Research Proposal
Strategies and Effectiveness of School-Based Education Session on Hand Washing Practices
hand hygiene is one of the first basic skills of patient safety that is taught to undergraduate nursing students.... hand hygiene is one of the first basic skills of patient safety that is taught to undergraduate nursing students.... hand hygiene is one of the first basic skills of patient safety that is taught to undergraduate nursing students.... As Boscart and McGilton (2008) note, both student's and healthcare providers' compliance with proper hand hygiene or handwashing is unacceptably low....
11 Pages
(2750 words)
Report
sponsored ads
Save Your Time for More Important Things
Let us write or edit the literature review on your topic
"Hand Hygiene and Infection Control"
with a personal 20% discount.
GRAB THE BEST PAPER

✕
- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY