StudentShare


Our website is a unique platform where students can share their papers in a matter of giving an example of the work to be done. If you find papers
matching your topic, you may use them only as an example of work. This is 100% legal. You may not submit downloaded papers as your own, that is cheating. Also you
should remember, that this work was alredy submitted once by a student who originally wrote it.
Login
Create an Account
The service is 100% legal
- Home
- Free Samples
- Premium Essays
- Editing Services
- Extra Tools
- Essay Writing Help
- About Us
✕
- Studentshare
- Subjects
- Health Sciences & Medicine
- The Interpretation of the Laboratory Test Results
Free
The Interpretation of the Laboratory Test Results - Case Study Example
Summary
This case study "The Interpretation of the Laboratory Test Results" focuses on an 86-year-old retired nurse, who saw her new GP after moving to Islington, because of repeated vomiting, nausea and generalized tiredness. Her prior history indicated similar problems about 4 months ago…
Download full paper File format: .doc, available for editing
GRAB THE BEST PAPER93.8% of users find it useful
- Subject: Health Sciences & Medicine
- Type: Case Study
- Level: Undergraduate
- Pages: 5 (1250 words)
- Downloads: 0
- Author: billybatz
Extract of sample "The Interpretation of the Laboratory Test Results"
Case Study Part A “I am very tired and started vomiting again”. Julie, an 86-year-old retired nurse, saw her new GP after moving to Islington, because of repeated vomiting, nausea and generalised tiredness for the last two weeks. Her prior history indicated similar problems about 4 months ago, where her previous GP referred her to the hospital. Julie underwent investigations at that time, including gastrointestinal endoscopy, blood tests showed no abnormality except for low serum sodium level (121 mmol/L), low blood glucose level (3.5 mmol/L) and relatively elevated serum potassium level (5 mmol/L). Further history questions reveal that Julie has no abdominal pain or alterations in her bowel movements. Julie is not on any medication and gives no history of allergies. Julie worked as a missionary in Kenya in the 1950’s. On examination, she looks unwell and drowsy. Her BMI is 22 and her vital signs are show in Table 1.
Table 1. Vital signs for Case Study
Julies results
Normal range
Blood Pressure (mmHg)
90/65
100/60-135/85
Pulse rate (beats/min)
100
60-100
Respiratory rate (breaths/min)
19
12-16
Temperature (oC)
37.2
36.6-37.2
Abdominal examination
Abdomen is soft and not tender or rigid Intestinal sounds are normal
No abdominal masses or organomegaly Old appendectomy scar is pigmented.
Cardiovascular and respiratory examinations are normal.
Neurological examination
Cranial nerves normal
No signs of meningitis or signs suggesting increased intracranial tension.
Answer
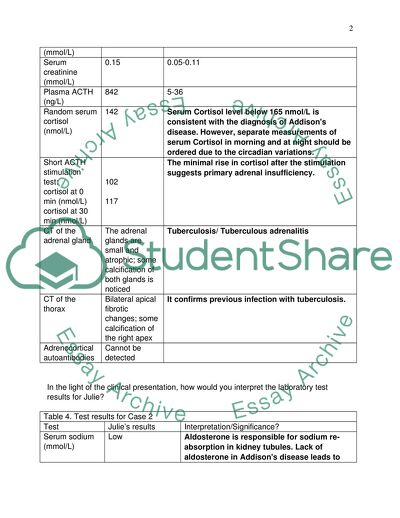
Table 2. Test results for Case 2
Test
Julie’s results
Normal range
Serum sodium (mmol/L)
123
135-145
Serum potassium (mmol/L)
5.8
3.5-5.0
Blood urea (mmol/L)
32
2.5-8.3
Serum creatinine (mmol/L)
0.15
0.05-0.11
Plasma ACTH (ng/L)
842
5-36
Random serum cortisol (nmol/L)
142
Serum Cortisol level below 165 nmol/L is consistent with the diagnosis of Addisons disease. However, separate measurements of serum Cortisol in morning and at night should be ordered due to the circadian variations.
Short ACTH stimulation test:
cortisol at 0 min (nmol/L)
cortisol at 30 min (nmol/L)
102
117
The minimal rise in cortisol after the stimulation suggests primary adrenal insufficiency.
CT of the adrenal gland
The adrenal glands are small and atrophic; some calcification of both glands is noticed
Tuberculosis/ Tuberculous adrenalitis
CT of the thorax
Bilateral apical fibrotic changes; some calcification of the right apex
It confirms previous infection with tuberculosis.
Adrenocortical autoantibodies
Cannot be detected
In the light of the clinical presentation, how would you interpret the laboratory test results for Julie?
Table 4. Test results for Case 2
Test
Julie’s results
Interpretation/Significance?
Serum sodium (mmol/L)
Low
Aldosterone is responsible for sodium re-absorption in kidney tubules. Lack of aldosterone in Addisons disease leads to hyponatremia.
Serum potassium (mmol/L)
Raised
Potassium is excreted in exchange for Sodium. Decreased Sodium re-absorption simultaneously accounts for decreased excretion of potassium which hence results in hyperkalemia
Blood urea (mmol/L)
Raised
Denotes impaired renal function. Dehydration resulting from vomiting and ionic imbalance is the cause.
Serum creatinine (mmol/L)
Raised
Denotes impaired renal function. Dehydration resulting from vomiting and ionic imbalance is the cause.
Plasma ACTH (ng/L)
Very high
Hallmark of primary adrenal insufficiency.
Random serum cortisol (nmol/L)
Low
Because of negative feedback inhibition by elevated ACTH.
Short ACTH stimulation test:
cortisol at 0 min (nmol/L)
cortisol at 30 min (nmol/L)
Blunted response
Failure of values to double after 30 minutes signifies the abnormality in adrenal glands indicating primary disease.
CT of the adrenal gland
The adrenal glands are small and atrophic; some calcification of both glands is noticed
Calcification shows the tuberculous aetiology whereas atrophy points towards chronicity of the infection.
CT of the thorax
Bilateral apical fibrotic changes; some calcification of the right apex
It is indicative of a previous exposure to tuberculosis which has led to these changes.
Adrenocortical autoantibodies
Cannot be detected
Rules out autoimmune adrenalitis. Also that there is no present infection and all the calcification might have been due to previous infections and exposure to microorganisms and diseases like tuberculosis.
c) What diagnosis do all of these factors lead to? Discuss the mechanisms underlying each cause and associated changes.
Answer: The clinical symptoms and the laboratory test findings of the patient lead to the diagnosis of primary chronic adrenal insufficiency, also known as Addisons disease after the name of Dr. Thomas Addison who first described the condition in 1855.The disease is associated with progressive destruction of the adrenal gland and ultimately, the loss of important hormones that are produced by the gland. Two important hormones, Cortisol and Aldosterone are produced by the adrenal cortex. They play a major role in bodys homeostasis, Aldosterone is the key regulator of electrolyte balance and Cortisol regulates the glucose metabolism and is the life saver especially in states of stress (like shock, hypotension). Being a steroid, Cortisol also exerts anti-inflammatory effects.
The symptoms of Addison’s disease do not become apparent unless 90% of the gland is destroyed and are usually nonspecific like fatigue, weakness and irritability. The case described here has a chronic presentation. There are a number of causes leading to this condition. By far, the most common cause is autoimmune adrenalitis (Autoimmune destruction of the adrenal cortex), which in this case can be ruled out right away as the laboratory results prove negative for adrenocortical antibodies. Another common cause of primary adrenal insufficiency is infections that affect the adrenal cortex, especially Tuberculosis, which in such cases is usually associated with or preceded by active tuberculous infection elsewhere in the body. Other infections can be those caused by Histoplasma or Coccidia and in immunocompromised patients having AIDS. Metastatic tumors from other organs sometimes involve adrenals, especially those from lungs and breast and destroy enough of the cortex to produce the symptoms of adrenal insufficiency. Apart from these, certain genetic disorders (like congenital adrenal hyperplasia) also produce primary adrenal insufficiency (Kumar et al 2005).
The present condition of Julie can be traced back to aldosterone dysregulation as the first imbalance, since aldosterone is the hormone that is first affected by the disease, followed by cortisol and androgens. Aldosterone is the hormone responsible for re-absorption of sodium in kidney tubules. Its deficiency results in the ionic imbalance (Guyton and Hall, 1996). Deranged sodium re-absorption leads to los of sodium in urine and its decreased levels in blood, i.e. hyponatremia. As a result, Potassium ions which are normally excreted in exchange for sodium from the body are retained resulting in hyperkalemia. The deranged glucocorticoid and mineralocorticoid activity also leads to persistent vomiting by disrupting the gastrointestinal ionic balance (ARLT et al 2006). There is no primary abnormality in the gastrointestinal tract as the endoscopy results were interpreted normal. The very high levels of Blood Urea and Creatinine are the result of severe dehydration resulting from persistent vomiting. The fluid derangement and impairment of the kidney functions lead to the increased levels of both these substances.
Measurement of plasma ACTH level is the key to diagnosis. Adrenocorticotropin hormone (ACTH) is produced by the Pituitary gland and stimulates the production of cortisol by adrenals. When cortisol levels are sufficient, ACTH secretion is inhibited by negative feedback mechanism. ACTH stimulation test which is the gold standard for primary adrenal insufficiency is performed to determine whether the abnormality lies in the adrenal gland or the pituitary (Boon and Davidson, 2006). Synthetic ACTH (Cosyntropin) is injected IV/ IM to the patient and the response is measured in terms of change in the cortisol levels. Normally, Serum and Urine cortisol levels should double the baseline after stimulation in 30 minutes. Rise in the level of cortisol proves that the abnormality lies in the pituitary. On the contrary, minimal or no change in cortisol level (as in Julies case) indicates the adrenal abnormality. As in this case of primary adrenal insufficiency, the pituitary function is normal and the decreased cortisol levels are due to atrophic adrenal glands which fail to produce ACTH even after the extrinsic ACTH stimulation. The atrophic glands seen on CT are characteristic of Addisons disease, while the calcification points to the tuberculous infection as its cause.
Hyperpigmentation of her appendix scar also points towards the abnormally high levels of ACTH which stimulate melanin production. Other signs and symptoms found on Julies physical examination as well as her vitals support the diagnosis of Addisons disease: Loss of Sodium leads to low blood volume resulting in hypotension, which explains the increase in respiratory rate. This, along with the generalized weakness caused by persistent vomiting leads to the unwell and drowsy appearance.
References
ARLT, W., ROSENTHAL, C., HAHNER, S., & ALLOLIO, B. (2006). ORIGINAL ARTICLE: Quality of glucocorticoid replacement in adrenal insufficiency: clinical assessment vs. timed serum cortisol measurements. Clinical Endocrinology. 64, 384-389.
BOON, N. A., & DAVIDSON, S. (2006). Davidsons principles & practice of medicine. Edinburgh, Elsevier/Churchill Livingstone.
GUYTON, A. C., & HALL, J. E. (1996). Textbook of medical physiology. Philadelphia, W.B. Saunders.
KUMAR, V., ABBAS, A. K., FAUSTO, N., ROBBINS, S. L., & COTRAN, R. S. (2005). Robbins and Cotran pathologic basis of disease. Philadelphia, Elsevier Saunders.
5. Top of Form
Top of Form
SMITH JC, SIDDIQUE H, & CORRALL RJ. (2004). Misinterpretation of serum cortisol in a patient with hyponatraemia. BMJ (Clinical Research Ed.). 328, 215-6.
Bottom of Form
Read
More
CHECK THESE SAMPLES OF The Interpretation of the Laboratory Test Results
Research Approaches and Methods
Historical research focuses on the narration and interpretation of past events.... The idealist school entirely uses experience and intuition as elements for interpretation.... The paper will discuss how Historical methods compare with five other methodologies, that is; case studies, experimental research methods, qualitative research methods, action research, and questionnaire-based surveys....
8 Pages
(2000 words)
Term Paper
Clinical Laboratory Improvement Act
In all events, tests, and devices, the user must strictly adhere to the manufacture's instructions in regards to the use, reading, and interpretation of the results.... CLIA is the Clinical Laboratory Improvement Act (Amendments), which sets the standards for the personnel, organization, accuracy, reliability, and auditing of medical testing as a means to assure that the testing of patients is uniformly implemented and the quality meets the guidelines, no matter where the test was administered....
5 Pages
(1250 words)
Assignment
Smooth Muscle Antigen
Different SMAs give different immunofluorescent staining patterns which help the laboratory to identify the SMA (Toh, 1979).... The history of the person for whom the ASMA test is being administered is of relevance in the conduct of tests and interpretation of results.... From the paper "Smooth Muscle Antigen" it is clear that the EIA test does not distinguish between acute, active, or resolved infection.... This could result in a 'false positive' test result....
4 Pages
(1000 words)
Research Paper
KFSH Reference Laboratory Services for Inherited Metabolic Diseases
ing Faisal Medical Laboratory offers a comprehensive laboratory test menu and will be the largest inherited metabolic Diseases laboratories in Saudi Arabia.... This paper presents Inherited Metabolic Disease laboratory which is a start-up service in addition to the existing King Faisal Medical reference laboratory (KFML) at King Faisal Specialist Hospital (KFSH) committed to providing the most convenient.... Other types of inherited laboratory testing not performed in-house will be sent to Mayo Medical laboratory as they have been identified as KFML reference laboratory....
25 Pages
(6250 words)
Research Paper
Quality Issues in the Analytical Laboratory
Software and computer systems used for acquisition, processing, recording, storage, and retrieval of test results need validation prior to use.... "Quality Issues in the Analytical laboratory" paper states that customer expectations can be fulfilled or even exceeded by opting for quality systems whether the organization concerned is a manufacturing industry or an analytical laboratory offering services of chemical analyses.... Fifield & Kealy (2000,p524) point out that a typical analytical laboratory carries out the development and day-to-day application of analytical methods in optimum conditions....
9 Pages
(2250 words)
Coursework
Interpretation of the Geophysical Data
This paper ''interpretation of the Geophysical Data'' tells that Geophysical data is collected at the field scale, but its accurate interpretation is made on the laboratory scale.... The measurement scale has significant impacts on the interpretation of geophysical data (Acosta-Colon, 2009).... Here, it is essential to notice that the composition and size of fluid-solid interface straightly influence the interpretations and different reactions in the laboratory setting....
6 Pages
(1500 words)
Article
Th Uss f Bihmil Dtin linil Mdiin
It further illustrates how analytical and biological factor affects biological test results and lastly, provides a relevant and accurate interpretation of normal and abnormal results with the use of relevance ranges to achieve clinical medicine decision-making inpatient management process.... Acquisition and interpretation of biochemical data mark a confidential diagnosis is based on the patient history and examination findings for characterization and recognition of the kind of the disease present with reference to clinical signs (Robinson, 2009)....
8 Pages
(2000 words)
Case Study
Clinical Biochemistry in Clinical Medicine
As a result, they have to liaise with the laboratory staff to acquire and use biochemical data.... This paper discusses the uses of biochemical data, acquisition, and interpretation.... The paper "Clinical Biochemistry in Clinical Medicine" explains the biochemical data is used for diagnosis, monitoring, prognosis, and screening goals....
6 Pages
(1500 words)
Literature review
sponsored ads
Save Your Time for More Important Things
Let us write or edit the case study on your topic
"The Interpretation of the Laboratory Test Results"
with a personal 20% discount.
GRAB THE BEST PAPER

✕
- TERMS & CONDITIONS
- PRIVACY POLICY
- COOKIES POLICY